Demystifying Symptoms and Promoting Recovery After a Concussion
As a neuropsychologist, I am fortunate to be in the position to assist children and adults in their recovery after brain injury by means of educational consultations, neuropsychological evaluations, and research.
Mild traumatic brain injuries (TBIs), in other words concussions, are a major public health issue in today’s youth, accounting for nearly 38% of pediatric emergency room visits. Many more go undiagnosed, particularly when there is no loss of consciousness.
Possibly related to the media’s recent focus on the potentially long-term, detrimental effects of sports concussion is the rapid growth in the demand for neuropsychological services post-concussion. Usually client referrals are presented to me when concussion symptoms, which initially were expected to have resolved in about 7 to 10 days, continue to linger and interfere with daily functioning.
While most individuals recover quickly and completely after concussion, a small proportion has ongoing symptoms that can be considered serious. Usually, a brief post-concussion evaluation is sufficient to identify areas of cognitive, emotional and social difficulties that have remained, and to provide educational resources and direction so that clients can be equipped to manage their symptoms, and improve their health and well-being.
Symptoms persisting beyond 3 months, while sometimes due to complications (i.e., numerous blows to the head rather than a single occurrence or positive findings on neuroimaging) can frequently be related to symptom expectation, stress and other psychological factors. Understanding the multiple causes of symptoms can be particularly important, as neurological findings alone may not explain why cognitive impairment (e.g., attention and memory problems) and physical symptoms (e.g., dizziness, headaches and sleep difficulties) persist even months after injury.
With emotional support and guidance, clients can gain perspective on their symptoms as well as clarity on how to resolve them. Even a single consultation session is typically sufficient to prevent post-concussion syndrome. Additional referral for medication, short-term psychotherapy, and cognitive training may be indicated.
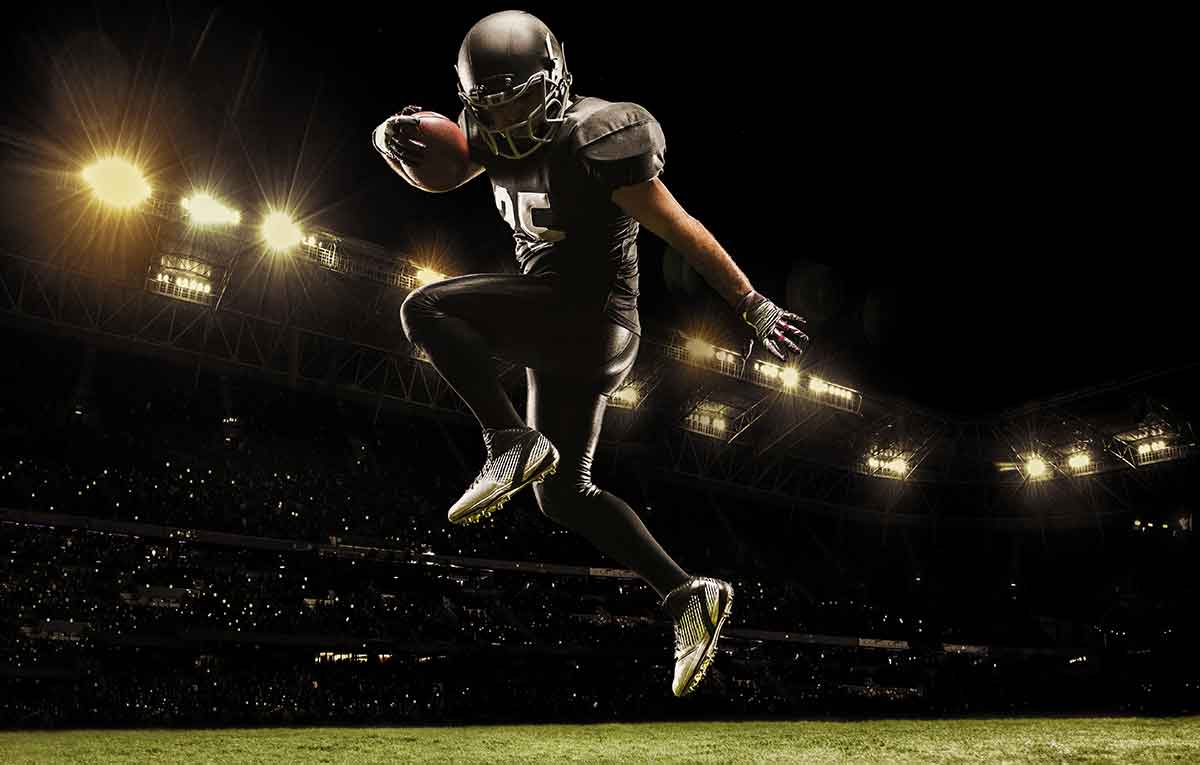
I actively engage in educating our community about the warning signs of concussion and help them follow appropriate measures before returning to school, work and sports. Concussion can be an inevitable consequence of participation in contact sports; however, understanding the recovery process in the young developing brain is challenging.
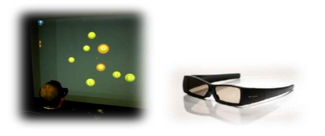
I have been collaborating with the Vancouver Island Concussion Team in exciting new research. Locally, Dr. Brian Christie has obtained baseline scores from a few hundred healthy minor hockey players using a 3-D perceptual training program (i.e., NeuroTracker, developed by Cognisens Inc. – see figure 1). This task is designed to reprogram the brain and boost performance in the real world, including how well athletes keep their eye on the ball while tracking where their multiple opponents are moving on the field.
Figure 1. Stages of the NeuroTracker Task
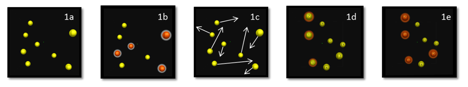
The subjects, ages 5-17, tend to be fascinated by this interactive computer game that can be played in either a 3-D immersion chamber or in front of a standard 3-D television. The object of the game is to visually track a set of four “target” balls with four “distracter” balls bouncing around the room competing for their attention. In the pilot study, performance for all adolescents was assessed over three blocks of 20 baseline trials.
We predict at least 10% of these young athletes will suffer a concussion over the next few years, and we will re-assess them if injured, along with testing additional youth solely post-concussion to better understand the capacity of the program to predict return to play status as well as the effects of concussion on visual-spatial skills. Thus far, significantly lower scores are noted post-concussion, and it is likely that return to baseline scores after repeated sessions are correlated to recovery.
Although Neurotracker has been established as a high tech means of cognitive training in healthy adult athletes including professional hockey players, soccer players, rugby and football players, we are beginning to utilize it as an assessment tool to better understand the recovery process post-concussion and to help us make more informed decisions such as when children have recovered enough cognitively in order to return to play.
Further, to ensure that evidence based techniques are used when working with my clinical populations, I am also involved in a Canadian Common Data Research Project with interest in collecting large scale mild TBI data from pediatric populations across the country. Our team of prominent scientist-practitioners, including Dr. Isabelle Gagnon, has been granted $1.4 million by the Canadian Institute of Health Research (CIHR) to study mild TBI in youth over the next 5 years, and we hope to collaborate with international projects, including European and American common data research teams funded by National Institutes of Health (NIH) for hopes of standardizing research, accelerating data collection, and arriving at a consensus on how concussion should be best assessed and managed.
It is expected that the generous support received will facilitate ongoing growth in the understanding of recovery post-concussion. I would personally like to send a special thanks to Dr. Judy Hall and the National Register in their ongoing support of my clinical work and research by means of the 2013 Early Career Psychologist Award, and the privilege of being included as the National Register’s first “Psychologist Spotlight.”